Critical care concepts are essential for the NCLEX-RN exam as they equip nurses with the knowledge and skills to manage life-threatening conditions. Understanding these concepts ensures safe, effective patient care, improving outcomes in high-stakes environments like ICU and emergency setting.
RESPIRATORY SYSTEM TUBES (Critical care concept)
Endotracheal tube (ETT): Needs Critical Care:
- Plastic tube inserted into the tracheal through the mouth or nose
- Maintains an airway to deliver oxygen and positive pressure to the lungs
- After placement of an ETT, placement should be verified by a chest x-ray
- Assess for equal breath sounds bilaterally
- The ETT can becomes displaced into the R main stem bronchus
- Ensure that breath sounds are heard equally bilaterally, or the tube may need to be repositioned
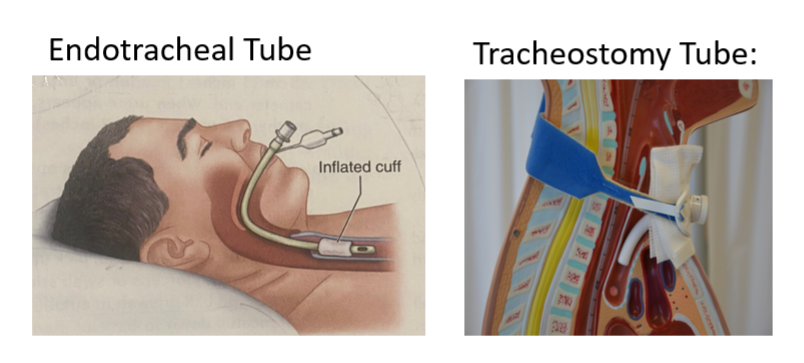
TRACHEOSTOMY TUBE: (Critical care needs):
- Nurse Must know:
- Infection prevention, the natural defenses of the nose and mouth are bypassed (higher risk for infection)
- Daily trach care
- Suctioning:
- Only suction to the pre-measured depth
- Suctioning too deep can cause damage or cause laryngospasm
- Don’t suction longer than 10 seconds
- Some clients may need pre-oxygenated with 100% FiO2
- Safety:
- You must keep two back up trachs at the bedside in case of emergency, 1 of same size and 1 a half size smaller.
- It the trach comes out, first try to insert the backup of the same size. If unsuccessful, try to insert the half size smaller.
Ventilators: (Critical care needs):
- The ICU nurse is caring for a sedated client on a ventilator. The ventilator alarm is beeping persistently for low pressure despite the fact the client is calm and has stable vitals. In that case, the most appropriate action for the RN to take first is to check the tubing for holes.
- If the patient’s presentation and vitals are stable, the nurse should check for any apparent equipment malfunction. If no air leaks or kinks are immediately identifiable, the nurse should call respiratory therapy or the rapid response team (RRT).
- Persistent alarms despite stable vitals may indicate the patient is trying to talk, or is developing a pneumothorax from increased intrathoracic pressure, or is biting/gagging on the endotracheal tube, or is experiencing bronchospasms. These alarms should never be ignored or turned off, as they may indicate early signs of a change in the patient’s condition.
| Pressure in the circuit is too high (HIGH) Ventilator alarm | Pressure in the circuit is too low (LOW) Ventilator Alarm |
| CAUSES: Client coughing Gagging Bronchospasm Fighting the ventilator ETT occlusion Kink in the tubing Increased secretions Thick secretions Water in ventilator circuit | CAUSES: Tubbing is disconnected Loose connections Leak Extubation Cuffed ETT or trach is deflated Poorly fitting CPAP/BiPAP mask |
Neurological Status: (Critical care concept)
- Intracranial Pressure:
- The pressure inside of the skull
- Normal = 5-15
- Causes of increased ICP:
- Tumor
- Bleeding
- Hydrocephalus
- Edema
- Signs and symptoms of Increased ICP:
- Headache: Often worse in the morning and exacerbated by activities that increase intracranial pressure, such as coughing or straining.
- Nausea and Vomiting: Especially vomiting that is sudden and without nausea (projectile vomiting).
- Altered Mental Status: Confusion, lethargy, decreased level of consciousness, and, in severe cases, coma.
- Papilledema: Swelling of the optic disc, visible upon eye examination.
- Visual Disturbances: Blurred vision, double vision (diplopia), and transient visual obscurations.
- Cushing’s Triad: Hypertension, bradycardia, and irregular respirations; a late sign indicating brainstem compression.
- Seizures: New-onset seizures can be a symptom of increased ICP.
- Pupil Changes: Unequal pupils (anisocoria) and sluggish or non-reactive pupils, indicating pressure on cranial nerves.
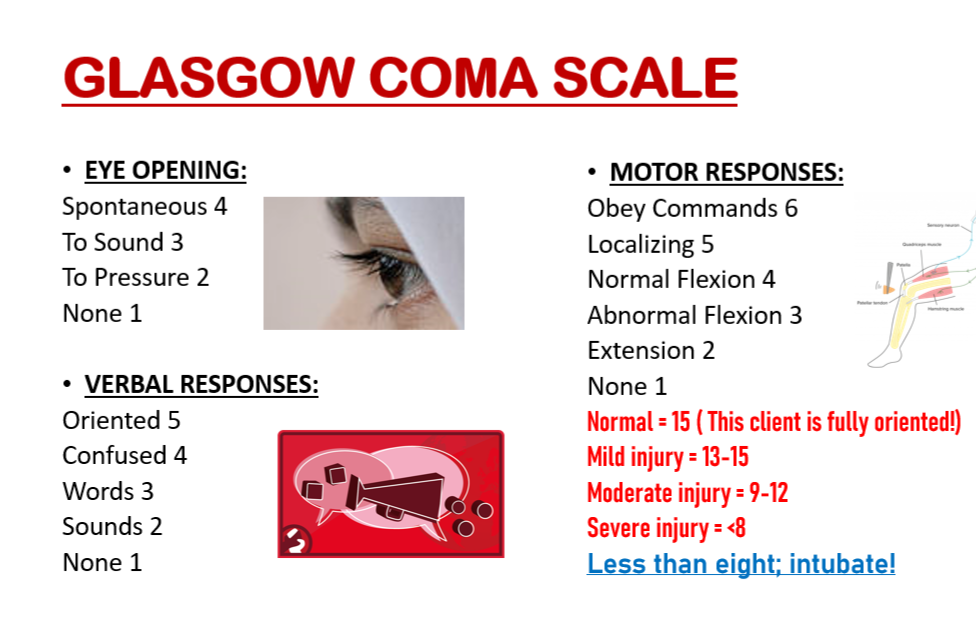
Glasgow Coma Scale
Glasgow Coma Scale Normal= 15
- Normal = 15
- This client is fully oriented!
- Mild injury = 13-15
- Moderate injury = 9-12
- Severy injury = <8
- Less than eight; intubate!
Decorticate and Decerebrate
- Posturing:
- Decorticate:
- Abnormal flexion
- Arms pulled in towards center
- Clenched fists
- Rigid muscles
- Damage to the midbrain
- Decerebrate:
- Abnormal extension
- Arms and legs straight out
- Toes pointed downwards
- Neck and had arched back
- Rigid muscles
- Damage to deep brain structures: pons
- Extension of the arms and legs indicates decerebrate posturing, an indication of increased intracranial pressure
Vasoactive Infusions: (Critical care concept):
Common Indications:
● Cardiac arrest
● Hypotension
● Shock refractory to fluid resuscitation
● Cardiac disease (Acquired or Congenital)
- Epinephrine
- Most often used in cold shock
- Low doses act on beta-1 receptors
- Increase the cardiac output
- High doses act on alpha-1 receptors
- Increase systemic vascular resistance → increase BP
- Norepinephrine
- Most often used in warm shock
- Acts on alpha-1 receptors
- Causes peripheral vasoconstriction → increases BP
- Increases cardiac output
- Dopamine:
- Used in trauma patients and cold shock
- Low doses used in kidney failure to increase renal blood flow (‘Renal dopa’)
- Low doses increase contractility → Increase CO
- Higher doses cause vasoconstriction → Increase SVR → Increase BP
- Phenylephrine:
- Used for anesthesia-induced hypotension
- Second line agent in some shock patients
- Only acts on alpha-1 receptors
- Causes only vasoconstriction – no inotropy
- Vasoconstriction → Increased BP
- Milrinone:
- Used in patients with:
- Cardiogenic shock
- Decreased cardiac output
- Congenital/acquired heart defects
- Causes systemic vasodilation, pulmonary vasodilation, decreased afterload, & increased contractility.
- Doesn’t increase oxygen consumption
- Used in patients with:
- Vasopressin:
- Antidiuretic hormone (ADH)
- ANTI-diuresis…. Less diuresis → more volume IN the vascular system.
- More volume → more pressure!
- Raises BP
- Second line in vasodilatory shock
- Third line in septic shock
- 1st: Dopa or Norepi
- 2nd: Epi or phenylephrine
- 3rd: Vaso
Total Parenteral Nutrition:
Total Parenteral Nutrition also called hyperalimentation
- Nutrition delivered intravenously
- Contains:
- Dextrose
- Amino acids
- Electrolytes
- Central line is preferred
- Indications of TPN:
- Enteral nutrition is contraindicated
- Client is not tolerating enteral nutrition
- High risk for aspiration
- GI tract obstruction
- Complications:
- Big infection risk. Scrub that hub! Wash your hands!! Gloves!!!
- Tubing is changed every day
- Refrigerated until ready to hang
- Fluid overload
- Hyper OR hypoglycemia
- Do not turn on or off suddenly
- Titrate
- Check blood glucose levels
- Embolism
Parenteral Nutrition is a form of nutrition and is used when there is no other nutritional alternative. Administering nutrition orally or through a nasogastric tube is usually initiated first, before PN is initiated.
TPN administered through a central vein. If the bag of intravenous solution of TPN is empty and the nurse is waiting for the delivery of a new bag of solution from the pharmacy, a 10% dextrose in water solution should be infused at the prescribed rate to prevent hypoglycemia.
Regular Insulin may be added to control the blood glucose level because of the high concentration of glucose in the parenteral nutrition solution.
Heparin may be added in PN to reduce the buildup of a fibrinous clot at the catheter tip.
Abrupt discontinuation of a PN solution can result in hypoglycemia. The flow rate should be decreased gradually when the PN is discontinued.
Complications of PN are Air Embolism, Hyperglycemia, Hypervolemia, Hypoglycemia, Infection, Pneumothorax.
Important point regarding PN
Important Critical care concepts or points you must know before giving your NCLEX-RN exam:
- A resuscitation (Ambu) bag needs to be kept at the bedside of a client with an endotracheal tube or a tracheostomy tube at all times.
- Never insert a plug (cap) into a tracheostomy tube until the cuff is deflated and the inner cannula is removed; prior insertion prevents airflow to the client.
- If the chest tube is pulled out of the chest accidently, pinch the skin opening together, apply an occlusive sterile dressing, cover the dressing with overlapping pieces of 2-inch (5cm) tape, and call the PHCP immediately.
- The airway is the priority concern in an inhalation injury.
- A client who is hypoxemic and has chronic hypercapnia may require low levels of oxygen delivery at 1 to 2L /minute. because a low arterial oxygen level is the client’s primary drive for breathing; always check PHCP’s prescriptions.
- A bag-valve resuscitation mask should be available at the bedside for all clients receiving mechanical ventilation.
- For all clients receiving mechanical ventilation, always assess the client first and then assess the ventilator.
- Never set the ventilator alarm controls to the off position.
- Clients with a respiratory disorder should be positioned with the head of the bed elevated.
- Acute cardiac tamponade can occur when small volumes (20-50mL) of fluid accumulate rapidly in the pericardium.
- For the client with Increased ICP, elevate the head of the bed 30-40 degrees, avoid Trendelenburg’s position, and prevent flexion of the neck and hips.
- Abrupt discontinuation of a PN solution can result in hypoglycemia. The flow rate should be decreased gradually when the PN is discontinued.
FREE PRACTICE MATERNITY RELATED QUESTIONS FOR NCLEX-RN 2024 – brandednurses