Have you know about the basic points of neurological system disorders. Here, I mentioned all the important points which as a nurse you must know…….multiple sclerosis, myasthenia gravis, Parkinson’s disease, Alzheimer’s disease…..
| CNS | PNS |
| BRAIN AND SPINAL CORD | PERIPHERAL NERVOUS SYSTEM |
| M.S. Multiple sclerosis | M.G. Myasthenia Gravis |
| Parkinsons | A.L.S Amyotrophic Lateral Sclerosis |
| Alzheimer | G.B. Guillain-Barre syndrome |
| Huntington disease |
BIG TEST TIP FOR THESE DISEASES:
No drugs and No interventions cure this condition.
We can only treat the progression.
PROMOTE INDEPENDENCE for all neuro disease patients.
TEACH NEVER DO ALL ADLs (activity of daily life)
GAIT training: First teach GAIT training, then offer CANE, then WALKER, last WHEELCHAIRMULTIPLE SCLEROSIS
M.S. MULTIPLE SCLEROSIS
Autoimmune disorder
● CNS inflammation
● Damages and degrades the myelin sheath surrounding neurons.
Memory trick:
MS: Myelin Sheath (destruction)
MS: Muscle spasm and stiffness
Teach the client:
a. BALANCE exercise and rest
b. AVOID 4 S's which trigger FLARE UPs
S- Stress (exercise, surgery, injury)
S- Sickness or Sepsis
S- Smoking
S- Sun and Extreme heat (hot tub, bath, sauna)
PHARMACOLOGY:
a. IVIG
b. Cyclosporin
MYASTHENIA GRAVIS
MYASTHENIA GRAVIS:
Communication between nerves and muscles destroyed.
MEMORY TRICK:
a. Dry-asthenia gravity
b. dry and weak body
c. body attack acetylcholine receptor, less acetylcholine=less secretion =end up with a dry body.
ASSESSMENT:
Weak muscles
Ptosis
Drooping eyelid
TEACH:
a. AVOID the 4'S= Trigger Flare ups.
Myasthenic crisis:
Intervention:
a. Airway protection (safety with swallowing)
Intubation set up - BED SIDE
Before meals: Give Pyridostigmine (anticholinesterase drug)
b. Encourage semi-solid fluid.
TREATMENT:
● Cholinesterase inhibitors
● Corticosteroids
● ImmunosuppressantsPARKINSON’S DISEASE
PARKINSON'S DISEASE:
Low DOPAMINE and High ACETYLCHOLINE
3 KEY SIGNS:
1. Shuffling gait and decreases arm swinging.
2. Pill rolling
3. Tremors at rest
Orthostatic hypotension
Akinesia
INTERVENTION:
● Fall risk
● No cure
● Therapy
PT
OT
SLP
● Carbidopa-levodopa.
Increase dopamine in the brain.
PHARMACOLOGY:
LEVODOPA & CARBIDOPA
Avoid PROTEIN
ALZHEIMERS
ALZHEIMERS:
Resulting in dementia that damage the brain.
Sign and sign: very forgetful and loss of reality
KEY POINT:
Protect these client as you protect child but treat them as an adult.
1. SAFETY: No rugs, LOCK everything.
2. LOCATION: Lock doors leading outside.
3. COMMUNICATION: Distract and REDIRECT from the reality. Do not present reality.
Alzheimer’s disease is the most common degenerative neurological illness and the most common cause of cognitive impairment. It is irreversible, progressing from deficits in memory and thinking skills to an inability to perform even the simplest of tasks.
When a client with Alzheimer’s disease becomes agitated, frustrated, or hostile, the nurse should respond in a calm and supportive way. Decreasing external stimuli is helpful. Touch can provide immediate security and reassurance. People with Alzheimer’s disease may become agitated or aggressive as the condition gets worse. Agitation may cause pacing, sleeplessness, or aggression.
Most of the time, agitation and aggression happen for a reason. When they arrive, try to find the cause. If you deal with the issue, the behavior may stop. For example, a person may have:
Pain, depression, or stress
Too little rest or sleep
Constipation
Soiled clothing
Sudden change in a well-known place, routine, or person
A feeling of loss—for example, the person may miss the freedom to drive.
Too much noise or confusion or too many people in the room
Being pushed by others to do something—for example, to bathe or to remember events or people—when Alzheimer’s has made the activity very hard or impossible.
Feeling lonely and not having enough contact with other people
Interaction of medicines
Nursing interventions for Alzheimer’s patients who are agitated include providing a safe environment that is free of external stimulation and offers calm, emotional support.
HUNTINGTON DISEASE
HUNTINGTON DISEASE:
Key point:
Passed on by genetics.
Only requires 1 parent.
Recommend Genetic counselling.
The cardinal features of Huntington’s disease include chorea (brief, involuntary movements involving the trunk, limbs, and face). Psychiatric symptoms such as depression, paranoia, delusions, and hallucinations are common with this disease. Weight loss is also a common finding caused by the excessive energy expended in abnormal movements.
Huntington’s disease is a neurodegenerative disease that is not well understood. This disease causes neuropsychiatric symptoms such as chorea, dystonia, abnormal eye movements, hallucinations, and weight loss.
Treatments include VMAT2 inhibitors such as tetrabenazine. Adjunctive treatments such as benzodiazepines may be utilized for symptoms such as uncontrolled chorea.
Performing range of motion exercises will help decrease the risk of further atrophy and should be encouraged. Huntington’s disease is a progressive condition that can lead to muscle atrophy and potential contractures. The patient in this situation should be given a program with range of motion exercises. The nurse can help the patient to increase his range of motion and prevent worsening of contractures by improving flexibility and reducing rigidity.
ALS: Amyotrophic lateral sclerosis
Key points:
Dysphagia: Difficult swallowing
Dysphasia: Difficult speaking
Priority finding: Increased respiration secretion.GUILLAIN-BARRE’ SYNDROME
GUILLAIN-BARRE' SYNDROME:
Respiratory failure: early signs:
Inability to cough
Inability to lift the head or eyebrows.
Guillain Barré is a polyneuropathy that is manifested by paralysis, paresthesia, autonomic disturbances, and depressed or absent reflexes. The paresthesia is typically found in the peripheral extremities and may persist for quite some time even after the return of motor function.
The nurse should recognize Guillain Barré quickly and ensure a patent airway as the ascending paralysis may impact the diaphragm. The cause of Guillain Barré can be certain pathogens such as Campylobacter jejuni, which may induce massive peripheral nerve demyelination. Other causes include certain immunizations and bone marrow transplantation.
IMPORTANT POINTS MUST KNOW:
- The upper cervical spinal nerves innervate the diaphragm to control breathing. Monitor all individuals with a spinal cord injury for respiratory problems, diaphragmatic breathing, and for diminished or absent reflexes in the airway (cough and gag). Until a cervical spinal cord injury can be excluded, the client should have immobilization via a cervical spinal cord collar.
- Respiratory rate is essential to monitor when a cervical spinal cord injury is sustained. The upper cervical spinal nerves innervate the diaphragm to control breathing. Thus, specific injuries to the cervical spinal cord could be catastrophic.
- A client experiencing status epilepticus will require aggressive treatment as this is a persistent seizure that continues to recur despite treatment or a seizure that has lasted more than five minutes. The RRT should be notified as this is a medical emergency and requires evaluation by the RRT team. Obtaining a prescription for a parenteral benzodiazepine such as lorazepam is appropriate and should be completed by the nurse. Benzodiazepines are key in terminating a seizure. Central to caring for a client with a seizure is, placing them on their side and loosening any restrictive clothing.
- Drug intoxication, from prescription or over-the-counter medications, is more common in the elderly due to slower metabolism and absorption. Combinations of digoxin, diuretics, analgesics, and anticholinergics should be examined.
AUTONOMIC DYSREFLEXIA
Autonomic dysreflexia (AD)
It is a condition in which your involuntary nervous system overreacts to external or bodily stimuli. It’s also known as autonomic hyperreflexia. This reaction causes:
A dangerous spike in blood pressure
Rapid heartbeat
Constriction of your peripheral blood vessels
Other changes in your body’s autonomic functions
The condition is most commonly seen in people with spinal cord injuries above the sixth thoracic vertebra, or T6. It may also affect people who have multiple sclerosis or Guillian-Barre syndrome and some head or brain injuries. AD can also be a side effect of medication or drug use.
AD is a severe condition that’s considered a medical emergency. It can be life-threatening and result in:
Stroke
Retinal hemorrhage
Cardiac arrest
Pulmonary edema
The symptoms of AD may include:
Sudden severe hypertension
Anxiety and apprehension
Irregular or racing heartbeat
Nasal congestion
High blood pressure with systolic readings often over 200 mmHg
A pounding headache
Flushing of the skin
Profuse sweating, particularly on the forehead
Lightheadedness
Dizziness
Confusion
Dilated pupils
TREATMENT:
1. Sit the client up to lower their BP
2. Antihypertensives
a. Hydralazine
3. Find the cause and treat
a. Full bladder? Cath
b. Constipated? Remove impaction!
c. Pressure injury? Reposition
d. Painful stimuli? Remove stimuli
e. Cold room? Change the temperature!
STATUS EPILEPTICUS
STATUS EPILEPTICUS:
Status epilepticus is a medical emergency. This is when a seizure has lasted five or more minutes. Additionally, status epilepticus is defined as repeated seizure activity over the course of thirty minutes. During an acute seizure, the nurse should place the client on their side, loosen restrictive clothing, and anticipate a prescription for a parenteral benzodiazepine such as lorazepam.
Status epilepticus requires more aggressive medical treatment, such as high-dose benzodiazepines or barbiturates.DELIRIUM
Delirium
It is an acute and reversible syndrome. It is characterized by changes in memory, judgment, language, mathematical calculation, abstract reasoning, and problem-solving ability. The most common causes of delirium are infection, medications, and dehydration.
Some symptoms of delirium include:
Hallucinations
Restlessness, agitation, or combative behavior
Calling out, moaning, or making other sounds
Being quiet and withdrawn — especially in older adults
Slowed movement or lethargy.
Disturbed sleep habits
Reversal of night-day sleep-wake cycleMENINGITIS
MENINGITIS
Inflammation of the spinal cord or brain.
CAUSED by a virus or bacteria.
Bacterial is more dangerous.
ASSESSMENT
● Nuchal rigidity
● Photophobia
● Kernig’s sign
● Brudzinski’s sign
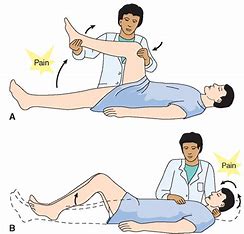 KERNIG's SIGN: The patient is in supine and the hip flexed at 90-degree; extension of the knee causes pain.
BRUDZINSKI's SIGN:
Brudzinski's sign is positive if passive flexion of the neck causes knee and hip flexion.
TREATMENT
● Steroids
● Analgesics
● Antibiotics - only if bacterial!!
● Isolation precautions
# Viral - contact precautions
# Bacterial - Droplet precautions
Bacterial meningitis is VERY contagious!! Medical emergency!!
# Prevention
Hib vaccine
Recommended for college students due to living in close quarters in dorm.
KERNIG's SIGN: The patient is in supine and the hip flexed at 90-degree; extension of the knee causes pain.
BRUDZINSKI's SIGN:
Brudzinski's sign is positive if passive flexion of the neck causes knee and hip flexion.
TREATMENT
● Steroids
● Analgesics
● Antibiotics - only if bacterial!!
● Isolation precautions
# Viral - contact precautions
# Bacterial - Droplet precautions
Bacterial meningitis is VERY contagious!! Medical emergency!!
# Prevention
Hib vaccine
Recommended for college students due to living in close quarters in dorm.Professional Nurse Practitioners: Top Nursing Programs for NP 2024 – brandednurses