Before moving to the gastrointestinal problem, first of all, I want to clear your few points regarding the normal levels of the liver and pancreas enzymes level.
- Normal AMYLASE levels are 60 – 120 Somogyi units/dL (100-300 u/L)
- Normal LIPASE levels are 0 – 160u/L (0 to 160 u/L)
- Increases value of Amylase and Lipase level indicate PANCREATITIS.
- Normal serum AMMONIA level = 10-80 mcg/dL (6-47 mcmol/L)
- The serum ammonia level assesses the ability of the liver to deaminate protein by products.
- Normal Liver enzymes levels:
- ALP: 38-126 u/L
- AST: 0-35u/L
- ALT: 4 – 36 u/L
- ALP: Alkaline phosphate
- AST: Aspartate aminotransferase
- ALT: Alanine aminotransferase
- Normal PROTHROMBIN time is 11 -12.5 seconds.
- Prothrombin time is prolonged with liver damage.
- Normal BILIRUBIN level is total 0.3 to 1.0 mg/dL
- An increase in bilirubin level indicates liver damage or bilirubin obstruction.
- LIVER:
- Largest organ
- Weight nearly 3 to 4 pounds.
- Contain Kupffer cells, remove bacteria in the portal venous blood.
- Remove excess glucose and amino acids from the portal blood.
- Secretes vitamins A, D, B & Iron.
- Secretes biles to emulsify fats (500-1000mL of bile/day)
- PANCREAS:
- MIXED GLAND
- Exocrine gland:
- Secretes sodium bicarbonate to neutralize the acidity of the stomach contents that enter the duodenum
- Endocrine gland:
- Secretes glucagon to raise blood glucose level.
- Secretes somatostatin to exert a hypoglycemic effect
- The Islets if Langerhans secrete INSULIN.
- STOMACH:
- Contains the cardia, fundus, body, and pylorus.
- MUCOUS GLANDS are located in the mucosa which prevent autodigestion by providing an alkaline protective covering.
- Hydrochloric acid kills microorganisms, break food into the small particles, and provides a chemical environment that facilitates gastric enzymes activation.
- Saliva contains the enzymes amylase (ptyalin), which aids in digestion.
DIAGNOSTIC PROCEDURES:
- BARIUM SWALLOW:
- Examination of the upper GI tract under Fluoroscopy after the client drinks barium sulfate.
- WITHHOLD FOODS & FLUIDS for 8 hours prior to the test. (PRE-PROCEDURE)
- LAXATIVE, INCREASE ORAL INTAKE FLUIDS, MONITOR STOOL for the passage of the barium. (Stools appear chalky white for 24 to 72 hours post procedure).
- Barium can cause a bowel obstruction.
- Following are the procedures in which patient should be NPO:
- Upper GI Tract study (Barium swallow) (8hours prior)
- Capsule endoscopy (3 hours before)
- Gastric analysis (12 hours prior)
- Upper GI ENDOSCOPY (6-8 hours prior)
- Fiberoptic colonoscopy (4 – 6 hours prior)
- ERCP (ENDOSCOPIC RETROGRADE CHOLANGIOPANCREATOGRAPHY): (6-8 hours prior)
- CT SCAN (At least 4 hours)
PEPTIC ULCER, TYPES, COMPLICATION, NURSING INTERVENTION
PEPTIC ULCERS.PEPTIC ULCER NCLEX POINT OF VIEW 1. Ulceration in the mucosal wall of the stomach, pylorus, duodenum, or esophageal in portions accessible to gastric secretions. 2. Common ulcers are GASTRIC & DUODENAL ULCERS. 3. ASSESSMENT OF GASTRIC ULCERS: a. Gnawing, sharp pain in or to the left of the mid epigastric region occurs 30 - 60 minutes after a meal (food ingestion accentuates the pain). b. Hematemesis is more common. 4. ASSESSMENT OF THE DUODENAL ULCERS: a. Buring pain occurs in the mid epigastric area 1.5 to 3 hours after a meal and during the night (often the awakens) b. Melena is common. c. Pain relieved by the ingestion of food. 5. CAUSES: same for both ulcers: Infection with H. pylori, stress, smoking, alcohol, use of corticosteroids, NSAIDS. 6.COMPLICATIONS OF GASTRIC ULCERS: Hemorrhage, Perforation, and Pyloric obstruction. 7.COMPLICATIONS OF DUODENAL ULCERS: Bleeding, Perforation, Gastric outlet obstruction, Intractable disease. 8. AVOIDS: Alcohol, caffeine, chocolate, smoking, aspirin, NSAIDS, corticosteroids.
| Interventions for Gastric ulcers | Interventions for Duodenal ulcers |
| Assess for vital signs and signs for bleeding. | Vital signs |
| Small, frequent bland feedings during active phase | Small, frequent bland feedings |
| H2 receptor antagonists or proton pump inhibitors to decrease the secretion of the gastric acid | Adequate rest |
| Antacids to neutralized gastric secretions. | Encourage the cessation for smoking. |
| Anticholinergics to reduce gastric motility | Antacids to neutralized gastric secretions. |
| Mucosal barrier protectants (1hours before each meal) | H2 receptor antagonists or proton pump inhibitors to decrease the secretion of the gastric acid |
| Prostaglandins for their protective and antisecretory actions | Treat H. Pylori |
| SURGERY: Total gastrectomy, Vagotomy, Gastric resection, GASTRODUODENOSTOMY (Billroth I), GASTROJEJUNOSTOMY (Billroth II), Pyloroplasty Postoperative complications: DUMPING SYNDROME, bleeding, diarrhea, hypoglycemia, Vit B 12 deficiency. | SURGERY: Done if ulcer is unresponsive to medications. |
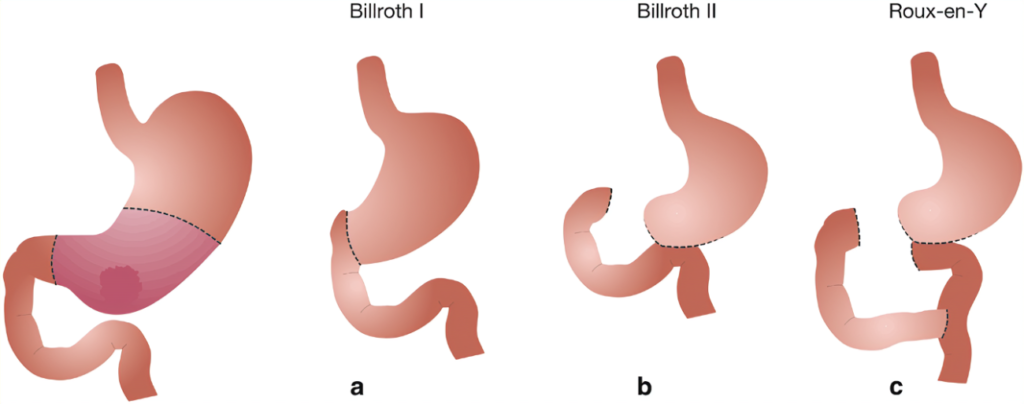
BILLROTH I AND II
Billroth I is also known as GASTRODUODENOSTOMY. Partial gastrectomy, with the remaining segment anastomosed to the duodenum.
Billroth II is also known as GASTROJEJUNOSTOMY: Partial gastrectomy, with the remaining the segment anastomosed to the jejunum
POSTOPERATIVE CARE:
Vital signs
Fowler's position
Administer fluid and electrolytes.
Assess bowel sounds.
Monitor NG SUCTION
Maintain NPO Status till peristalsis return.
Progress the diet from NPO to sips of clear water to 6 small bland meals a day.
Monitor for complication Dumping syndrome.DUMPING SYNDROME:
Dumping syndrome is the rapid emptying of the gastric contents into the small intestine that occurs gastric resection. Symptoms occurring 30 minutes after eating.
BORBORYGMI is the loud gurgling sounds resulting from bowel hypermotility seen in this syndrome.
Avoid sugar, salt, milk.
Eat high protein, high fat, low carbohydrate diet, LIE DOWN AFTER MEALS, take ANTISPASMODIC medications as prescribed to delay gastric emptying.
Following the gastric surgery, DONOT IRRIGATE OR REMOVE THE NG TUBE unless specifically prescribed because of the risk for disruption of the gastric sutures.
LIVER CIRRHOSIS
NCLEX POINT OF VIEW
LIVER CIRRHOSIS
A chronic, progressive disease of the liver characterized by the diffuse degeneration and destruction of the hepatocytes.
Repeated destruction of hepatic cells causes the formation of scar tissue.
The most common causes are chronic hepatitis C, alcoholism, nonalcoholic fatty liver disease, and nonalcoholic steatohepatitis.
COMPLICATIONS:
Portal hypertension: increase in pressure in the portal vein.
Ascites: accumulation of fluid in the peritoneal cavity result from venous congestion of the hepatic capillaries.
Bleeding: Fragile, thin walled, distended esophageal veins that become irritated and rupture.
Coagulation defects: Decreased synthesis of bile fats in the liver prevents the absorption of fat-soluble vitamins, without vitamin K and clotting factors II, VII, IX, and X prone to bleeding.
Jaundice: liver is unable to metabolized bilirubin.
Portal systemic encephalopathy : Altered level of consciousness, neurological symptoms, impaired thinking, neuromuscular disturbances.
Hepatorenal syndrome: Dec. urine output, Elevated BUN & Creatinine levels, Dec. urine sodium excretion, increased urine osmolarity.
Assessment:
Caput medusae (dilated abdominal veins)
Ecchymosis; petechiae
Jaundice, Pale, Plamer edema,
Chest angiomas,
Gynecomastia
Dyspnea
Ascites
Hypocalcemia, hypokalemia,
cardiac dysrhythmias, portal hypertension
Anemia, impaired coagulation, ASTERIXIS (FLAPPING TREMOR), Ascites, Clay-colored stools.
INTERVENTIONS:
Elevate the head of the bed to minimize shortness of breath.
Provide supplement!
Restrict sodium intake, fluid intake,
Initiate enteral feeding or parenteral nutrition.
Administer diuretics, monitor intake and output, Monitor LOC, asterixis, fetor hepaticus (fruity, musty breath odor of severe chronic liver disease.
Maintain gastric intubation to assess bleeding.
Administer blood products.
Coagulation Lab test check
Antacid prescribed.
Administer LACTULOSE (dec. pH of the bowel)
Avoid medications such as opioids, sedatives, barbiturates, hepatotoxic medications or substances.
Paracentesis preparation.GASTROINTESTINAL MEDICATIONS
ANTACIDS
1. React with gastric acid to produce neutral salts or salts of low activity
2.Used for peptic ulcer disease &
NCLEX TIPS: ANTACIDS
1. Anti-acids NEVER MIX with another Medicine.
2. Anti-acids do not last long.
3. Acronym "SCAM"
S: Sodium Bicarbonate (brand: Alka-Seltzer)
C: Calcium Carbonate (Brand: Tums, Rolaids)
A: Aluminum Hydroxide
M: Magnesium Hydroxide (brand: Milk of Mag.)
4. Aluminum and Calcium causes CONSTIPATION.
5. Magnesium cause DIARRHEA
6. Magnesium hydroxide can upset stomach and liquid bowel movement.
7. Not for heart failure patient because they contain sodium which swells the heart.
H2 BLOCKERS
1. "tidine"
2. RaniTIDINE (Zantac)
3. FamoTIDINE (Pepcid)
4. Key point: 30 minutes before the meal
5.Given for ulcers, GERD,
6. Big patient Education:
a. No overeat.
b. No stress
c. No smoking
d. No NSAIDS because it leads to GI bleeding.
PPI
PROTON PUMP INHIBITORS:
1. Ending in " -PRAZOLE"
2. Omeprazole (Prilosec)
3. Esomeprazole (Nexium)
4. Pantoprazole (Protonix) Famous
5. Key points: 3P's
6. Prevent holes: "stress ulcer prophylaxis."
7. Porous Bones " regular bone density test".
8. Possible GI infections "C- Diff"
9. INDICATIONS: Heart burns, GERD, Ulcer prophylaxis.
10. Prevents development of ulcer due to surgery or hospital stays.
11. Works by reducing the gastric acids by inhibiting the proton pump in the parietal cells of the stomach.
12. Increasing the risk for osteoporosis with long term use (Bad thing), increasing the risk for fractures on the spine, wrist, and hip so, always take CALCIUM and VIT-D.
13. It suppresses the normal HCL in the stomach which normally control the intestinal bacteria.
14. Key point: Take 30 minutes before the meals.
MUSCLE PROTECTANT
SUCRALFATE
1.Brand name is Carafate
2. Given to treat and prevent both stomach and duodenum or duodenal ulcers in the small intestines.
3. Mode of action: I t forms a thick protective layer over the ulcer provides a physical barrier against the stomach acids and enzymes so it's kind like a band-aid over an open wound.
4. Food and Medicines at least 1-2 hours before and after taking med.
5. Empty stomach take
6. Do not take with any other medicine.
MEMORY TRICK:
SUCRALFATE: 2 HOURS before you ATE, Taken LATE (best at bedtime).
MEDICATIONS TO TREAT INFLAMMATORY BOWEL DISEASE:
Inflammatory bowel disease has 2 forms, “Crohn’s disease and Ulcerative colitis.”
Ulcerative colitis: 15-20 stools severe diarrhea that may contain blood and mucus.
Crohn’s disease: Diarrhea semisolid, which may contain pus and mucus.
1. Antimicrobials {Ciprofloxacin, Metronidazole, Rifaximin, Clarithromycin}
2. 5-Aminosalicylates "zine" {Sulfasalazine, Olsalazine}
3. Corticosteroids "sone" {Prednisone, Hydrocortisone}
4. Immunosuppressants "prine" {Azathioprine, Cyclosporine}
5. Immunomodulators "mab" {Adalimumab, Certolizumab, Infliximab, Natalizumab}